Blog post by Erika Lassig
Picture your football final. The score is close, there’s less than two minutes on the clock and if your team makes one more try you’ll be the champions. You see an opening in the defensive line, a chance to make the winning try. Your teammate sees it too and passes you the ball. You make your play. You get tackled close to the line but make it over and get that winning try. But on your dive to the ground your stretch out your hand to brace your body against the fall. You feel something snap in your wrist when you hit the ground but at the first the adrenaline blocks out any pain.
Embed from Getty Images
A few hours later the pain bites as your turn on the tap for the shower. It starts to ache and you can’t sleep. You take some Nurofen, ice it and go to bed. The next morning it’s a little bit swollen and sore but the pain is manageable and it only really hurts when you turn on a tap or grip something. You think “if it was broken it wouldn’t be able to move it at all, must be just a sprain”. After a supposed wrist sprain, many people ignore it and carry on, assuming it will heal. But wrist sprains can be serious. What you do next could be critical to the long-term health of your wrist joint.
Did you know that the wrist joint involves 15 bones with many ligaments joining these bones to each other? Ligaments are pieces of tough tissue that join bone to bone providing stability to joints. This makes the wrist arguably the most complicated joint in the human body. A sprain is an injury to one or more of these ligaments. A fall on an outstretched hand can cause a fracture to any one of these 15 bones, a sprain to some of the ligaments, and/or a dislocation to one of the joints. And the scary part is that a fracture or serious sprain doesn’t always hurt as much as you would expect.
Embed from Getty Images
For this reason, if your wrist hurts after a fall, it’s vitally important to see a doctor to get an x-ray. A neglected injury can lead to an unstable or painful joint for years to come. Apart from identifying any factures, x-rays can also show any unusual positioning of the bones that may indicate a torn ligament. While it’s encouraging if the x-ray comes back clear, it doesn’t mean you’re out of the woods. Some fractures of the small carpal wrist bones, particularly the scaphoid, are difficult to see on x-ray. Depending on the site of the pain, your GP may recommend another x-ray in a few days or a CT or MRI scan. These other scans can be expensive and not always required in the outset so don’t worry if your doctor doesn’t recommend one.
So, your x-ray shows no fracture, the swelling has gone but your wrist still hurts sometimes. Is it best to wait it out or get treatment straight away? My advice to you is that you should get treatment straight away, as you are likely to recover faster. But it’s important that you see the RIGHT person. Someone who knows wrist injuries and has lots of experience treating them. You can be sure to find someone with the appropriate experience if they are a member of the Australian Hand Therapy Association, soon to be known as an Accredited Hand Therapist. This is an occupational therapist or physiotherapist with additional training and extensive experience managing hand, wrist and elbow injuries. You can find an appropriate therapist here https://www.ahta.com.au/site/find-a-therapist.
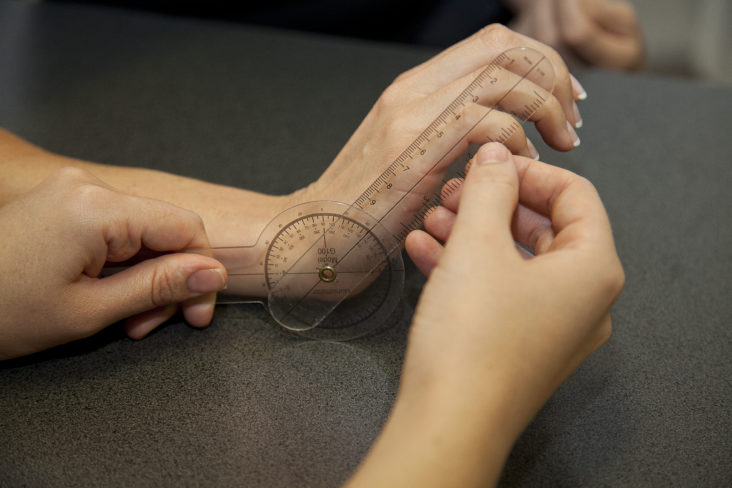
Once you’ve booked an appointment with an experienced practitioner in hand therapy, ensure you take any x-rays or scans that you have to your appointment. At your initial appointment, you can expect a thorough wrist and hand assessment. This helps to identify which ligament you have injured and how severe the damage may be, particularly if you haven’t had an MRI. Correct diagnosis allows you and your therapist to develop an appropriate treatment plan. We can help you to understand the role of the injured structures in your wrist and why you should follow our advice for splinting, bracing or taping, activity restriction and therapy exercises.
The two most commonly injured ligaments in the wrist are the triangular fibrocartilage complex (TFCC) and the scapho-lunate ligament (SLL). These ligamentous structures have vastly separate roles and therefore they shouldn’t be treated in the same way.
The TFCC is a group of three ligaments and a cartilage pad. It plays a vital role in stabilising the part of the wrist that performs rotation of the forearm. An injury to the TFCC often causes pain on the little finger side of the wrist, particularly with twisting (such as turning taps) or gripping.
The scapho-lunate ligament has two parts and joins two of the small carpal bones of the wrist: the scaphoid and the lunate. This ligament is very important in making sure the wrist bones move the way that they were designed. An undiagnosed injury to the SLL may lead to serious wrist problems in the future. This injury causes pain in the middle of the wrist with gripping and when leaning on the hand.
After initial assessment to get a diagnosis, several therapy sessions will be required to monitor your recovery and progress your treatment. A custom-made orthosis or semi-rigid wrist splint may be required to rest the injury to allow healing. Gentle and very specific exercises will likely be started early in your rehabilitation and these will change and increase over time. You may also be given some unusual exercises such as using water in bottles or pipes or even rolling marbles on plates!
The most important thing is to get qualified treatment early, follow your treatment guidelines and commit to your recovery plan by dutifully doing prescribed activities and exercises or avoiding restricted activities. It just might be the difference between a full recovery and partial recovery. For more articles like this, like our Facebook page https://www.facebook.com/thehandrecoverycentre/ or visit our website for more details https://www.handrecovery.com.au/what-is-hand-therapy/ .